

How Does the Menstrual Cycle Influence Bone Health?
We chat with Dr. Kate Ackerman to explore the relationship between low energy availability, menstrual cycles, and bone health.
June 26, 2024

Kate Ackerman, MD, MPH
Dr. Kate Ackerman is Director of the Wu Tsai Human Performance Alliance Female Athlete Program, an Attending Physician in the Orthopedics and Sports Medicine Department at Boston Children’s Hospital, Associate Professor of Medicine at Harvard Medical School, Co-Chair of the U.S. Olympic and Paralympic Committee’s Women’s Health Task Force, and Chair of the U.S. Rowing Medical and Sports Science Committee.
In athletics, stories of success often overshadow the struggles that lurk beneath the surface. Take Mary Cain, a promising athlete who rose through the ranks in 2013 to join Nike’s prestigious Oregon Project, considered the world’s premier track team at the time. Behind the facade of success, there was a troubling reality. After restrictive dieting and pressure from her coach, Mary Cain shared with the New York Times that she lost her menstrual period for three years and broke five bones.
Her experience underscores a common pitfall in striving for peak performance. We often focus on visible signs of progress, like muscle growth or speed, while overlooking more elusive players in our health, such as our bones. Unlike muscles, we can’t see our bones getting stronger, which makes prioritizing their health more challenging. To keep our bones healthy and safely reach our performance goals, our hormones play a vital role.
The Role of Estrogen in Bone Health
Bone is living, dynamic tissue that continuously grows and changes – and estrogen plays a vital role in its health.1 Estrogen helps the body absorb more calcium from the food we eat and slows down the activity of osteoclasts, the cells that break down bone.2,3,4 Without enough estrogen, these cells can become more active, causing bone loss and potentially contributing to bone stress injuries that take months to heal.5
Why would an athlete lack estrogen? Whether intentional or not, athletes can end up in a state of low energy availability.6 Low energy availability is when you don’t eat enough to cover your exercise and bodily function energy needs, and your body begins to prioritize vital organs like the heart and lungs.
“As a result, less critical physiological systems – such as the reproductive system – may shut down,” said Dr. Kate Ackerman. “There’s a drop in estrogen and other important hormones, which are then not available for bone.”6,7

Canva Pro Images

Training Tip
Adequate nutrition, exercise, and lifestyle habits are crucial for supporting bone health, with calcium, vitamin D, iron, and weight-bearing, multi-directional exercise playing significant roles.1,8,9,10,11
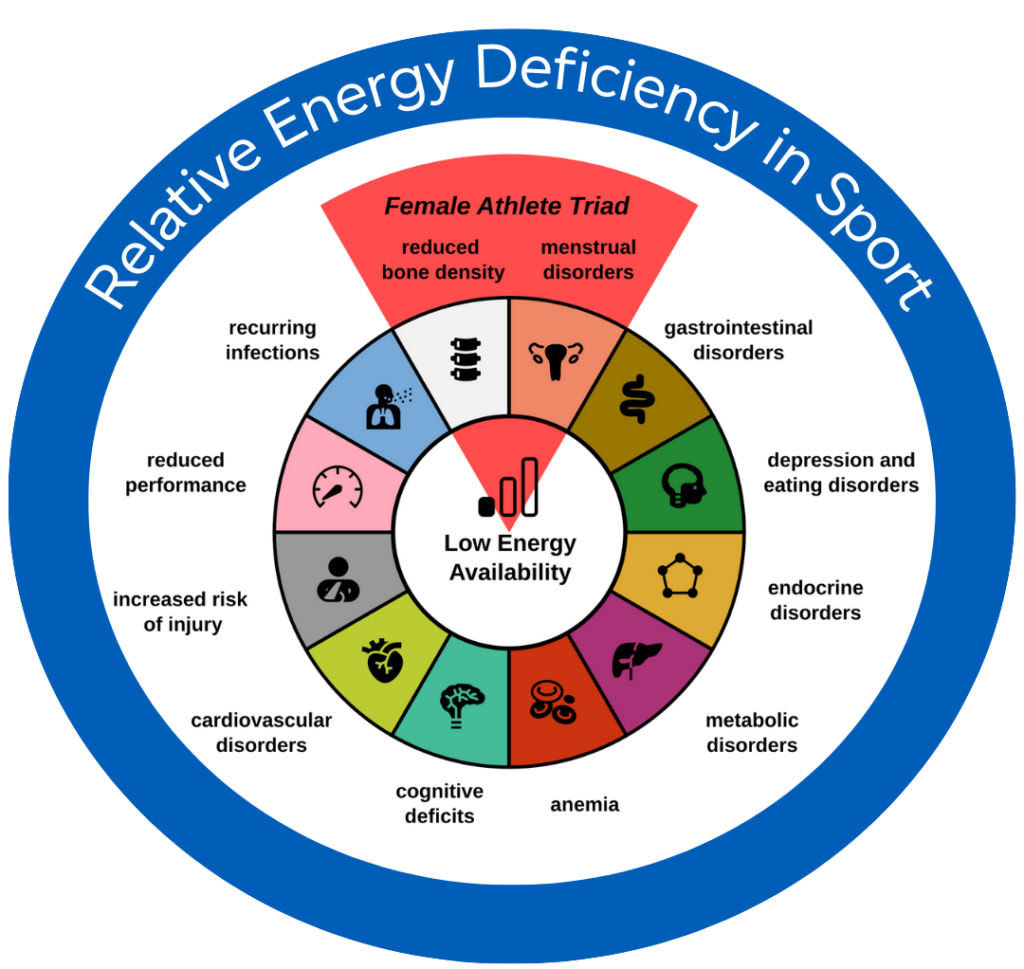
Menstrual cycle irregularity is a symptom that doctors can track and connect to a person’s bone health. “If someone isn’t eating enough, they might lose their period, and then they can have low bone density,” said Dr. Ackerman. “This is the original ‘Female Athlete Triad’ that was first discussed in the early ‘90s.”1,7
“The scientific community has now moved on from the original Female Athlete Triad to ‘Relative Energy Deficiency in Sport’ (REDs), recognizing that hormonal imbalances impact many different body systems,” added Dr. Ackerman.6 Athletes with REDs may also experience other changes to the body, such as cardiovascular dysfunction and metabolic disturbances.
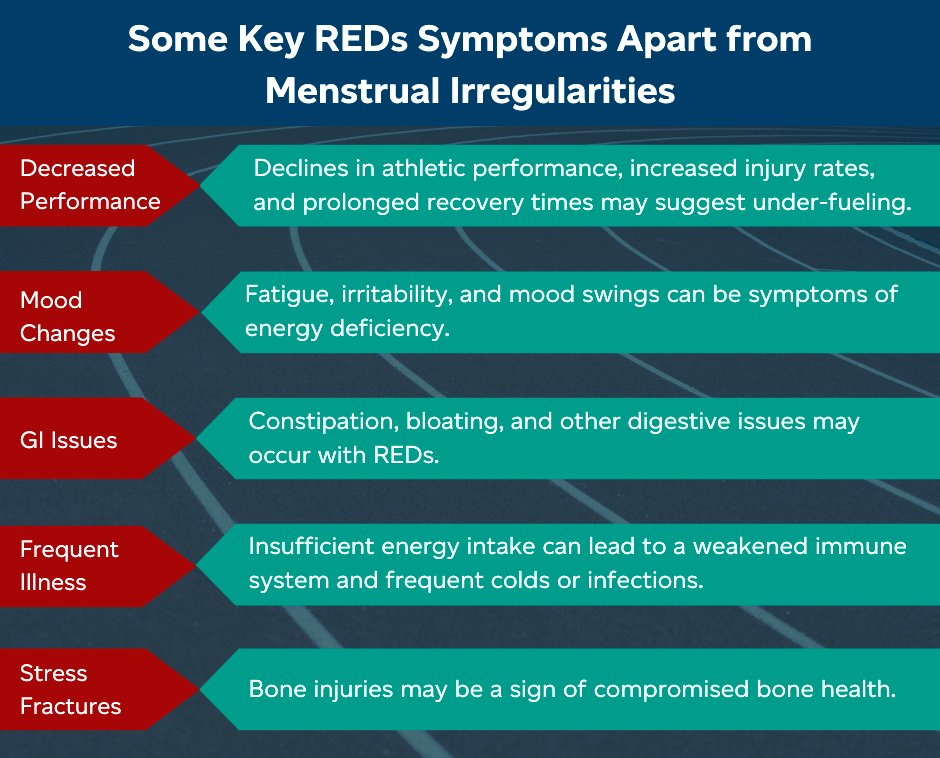
“Your missed period is one indication that you’re under-fueling, but it’s not the only one,” said Dr. Ackerman. “You can be under-fueling and still get your period.”
Researchers are still trying to understand why the order in which body systems are affected varies among individuals. For example, one person might experience muscle fatigue or cognitive changes before noticing menstrual irregularities. “This is an area of research that is ongoing,” added Dr. Ackerman.
MaligneRange/Wikimedia Commons CC BY-SA 4.0
Did You Know?
While estrogen is a primary hormone to support bone health, it’s not the only one. “There are also about 15-20 hormones that are necessary,” said Dr. Kate Ackerman.2,12,13
Signs of REDs Beyond a Missed Period
The body’s response to low energy availability varies among individuals and is influenced by many factors, including genetics. Recognizing REDs involves identifying a combination of symptoms and risk factors.6
If you’re uncertain if you have REDs, consult a doctor who specializes in sports medicine or endocrinology. They may assess your dietary intake, recommend a DXA scan to measure bone mineral density, and request blood tests to evaluate levels of key hormones like estrogen, cortisol, and thyroid hormones.
Keep in mind that you don’t need to have an eating disorder to develop REDs; you may simply be unaware you are not getting enough nutrients to fuel your training.
Resources for Athletes: Understanding and Preventing REDs
Relative Energy Deficiency in Sports (REDs) negatively impacts many systems in the body, such as energy metabolism and musculoskeletal health, which can lead to an increased risk of injury and decreased sports performance.6 REDs can also affect athletes of all ages, sports, and genders. Screening and prevention strategies are important for athletes to better understand their bone health. Check out RED in Sport and Stanford’s Female Athlete Science and Translational Research (FASTR) program to learn more.
Debunking the Myth: Energy Deficiency and Hormonal Treatments
Hormonal replacement therapies are sometimes used to address bone mineral density issues. The efficacy of various treatments for improving bone health is a topic for another article, but they shouldn’t be seen as a complete solution.
“Hormonal replacement therapies are only a band-aid solution to the bone problem while you’re trying to fix the energy deficit,” said Dr. Ackerman. If you’re in an energy deficit, your body still won’t have the necessary resources to support all its systems properly.
To truly protect your bone health, you need to ensure you’re consuming enough nutrients to meet your body’s needs. A pill or patch with estrogen isn’t sufficient. Other activities like weight-bearing, multi-directional exercise also play a significant role.1,8,9,10

Canva Pro Images
Did You Know?
When you experience bleeding while using oral contraceptive pills (OCPs), you’re not experiencing menstruation. It’s called withdrawal bleeding, which is usually briefer and lighter than your typical menstruation, where the thickened uterus lining is shed. Taking exogenous hormones, like the ones in OCPs, downregulates your natural hormones and the withdrawal bleed while on OCPs is the result of the drop of the exogenous hormones during the placebo week.14,15
Dr. Ackerman highlights that everyone is different, and you may need to find a personalized approach for bone health that works best for you. Consult with an expert to ensure you are getting enough energy intake to meet your energy demands.
To learn more about bone health, read our Playbook article “Start ‘Em Young: Prevention of Bone Stress Injuries in Athletes.”
Get Deeply Researched Insights on Human Performance
Join our mailing list to get actionable performance tips and nuanced explanations of the science.

Flash Q&A with Dr. Kate Ackerman
How do you like to stay active?
I’m a rower, so that will always be my favorite athletic activity. Fall rowing on the Charles River in Boston is my happy place.
What future developments in the field are you excited about?
I’m excited about understanding the pathways better. Studying different populations, affecting their energy availability, and seeing what markers change so that we have more markers to use to help our athletes monitor their health.
What sports are you excited to watch at the Olympics?
Rowing, of course! I’m the lead doctor for the U.S. Rowing Team and will be with them in Paris. I also look forward to seeing so many other events- swimming, track and field, gymnastics. It’s such a privilege to care for the athletes and to be there to experience it all.
Citations
- Hoenig, T., Ackerman, K.E., Beck, B.R., et al. (2022) Bone stress injuries. Nature Reviews Disease Primers. 8(26). https://doi.org/10.1038/s41572-022-00352-y
- Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004.
- Noirrit-Esclassan E, Valera M-C, Tremollieres F., et al. (2021). Critical role of estrogens on bone homeostasis in both male and female: from physiology to medical implications. International Journal of Molecular Sciences. 22(4): 1568. https://doi.org/10.3390/ijms22041568
- Almeida M., Laurent M. R., Dubois V, et al. (2016) Estrogens and androgens in skeletal physiology and pathophysiology. Physiological Reviews. 97(1):135-187. https://doi.org/10.1152/physrev.00033.2015
- Bishop M. E., Ahlmen A., Rosendorf J., et al. (2021) Bone stress injuries in female athletes. Annals of Joint. 6(2415-6809). https://doi.org/10.21037/aoj.2020.04.04
- Mountjoy M., Ackerman K.E., Bailey D.M., et al. (2023) International Olympic Committee’s (IOC) consensus statement on Relative Energy Deficiency in Sport (REDs). British Journal of Sports Medicine. 57(17):1073-1097. https://doi.org/10.1136/bjsports-2023-106994
- Ilich, J. Z., Kerstetter, J. E. (2000). Nutrition in bone health revisited: a story beyond calcium. Journal of the American College of Nutrition. 19(6): 715–737. https://doi.org/10.1080/07315724.2000.10718070
- Areta J.L. , Taylor H.L. , Koehler K. (2020) Low energy availability: history, definition and evidence of its endocrine, metabolic and physiological effects in prospective studies in females and males. European Journal of Applied Physiology. 121:1–21. https://doi.org/10.1007/s00421-020-04516-0
- Tenforde A.S., Fredericson M. (2011) Influence of sports participation on bone health in the young athlete: a review of the literature. 3(9): 861-867. https://doi.org/10.1016/j.pmrj.2011.05.019
- Fredericson, M., Ngo, J., Cobb, K. (2005) Effects of ball sports on future risk of stress fracture in runners. Clinical Journal of Sport Medicine. 15(3): 136-141. https://doi.org/10.1097/01.jsm.0000165489.68997.60
- Ackerman, K. E., Holtzman B., Cooper K. M., et al. (2019). Low energy availability surrogates correlate with health and performance consequences of Relative Energy Deficiency in Sport. British Journal of Sports Medicine. 53:628-633. https://doi.org/10.1136/bjsports-2017-098958
- Elliott-Sale, K. J., Tenforde, A. S., Parziale, A. L., et al. (2018) Endocrine effects of relative energy deficiency in sport. International Journal of Sport Nutrition and Exercise Metabolism. 28(4): 335-349. https://doi.org/10.1123/ijsnem.2018-0127

Does REDs affect male athlete bone health similarly as in female athletes?
As the Elliott-Sale publication highlights, fewer studies have examined the effects of low energy availability on bone mass density, bone quality, and bone metabolism in male athletes than females, and the results of these studies are less conclusive.
- Mills E.G., Yang L, Nielsen M.F., et al. (2021) The relationship between bone and reproductive hormones beyond estrogens and androgens. Endocrine Reviews. 42(6):691-719. https://doi.org/10.1210/endrev/bnab015.
- Ackerman K. E., Singhal V., Baskaran C., et al. (2019) Oestrogen replacement improves bone mineral density in oligo-amenorrhoeic athletes: a randomised clinical trial. British Journal of Sports Medicine. 53: 229-236. https://doi.org/10.1136/bjsports-2018-099723
- Ackerman K. E., Singhal V., Slattery M., et al. (2020) Effects of estrogen replacement on bone geometry and microarchitecture in adolescent and young adult oligoamenorrheic athletes: a randomized trial. Journal of Bone and Mineral Research. 35(2): 248-260. https://doi.org/10.1002/jbmr.3887
Playbook Terms of Use & Copyright
©2023-2024



