Exercise helps shape macrophage response for improved immune health
Collaborators
After a tough workout, you might feel sore the next day – this is a form of short-term inflammation. But over time, we also see that regular exercise is associated with lower chronic inflammation. How can we explain this apparently contradictory influence of exercise on inflammation? A study from UC San Diego provides a deeper understanding of how this happens at the cellular level, focusing on a key immune process known as macrophage polarization.
Macrophages are immune cells essential for fighting infections and repairing tissue. Polarization is the process by which macrophages adopt distinct functional states in response to signals from the environment. Exercise may serve as a key signal in this process, helping to explain some of the health benefits of regular physical activity.

Canva Pro Images
There are two primary states of macrophages: M1, which triggers pro-inflammatory responses to combat infections, and M2, which promotes anti-inflammatory tissue repair. How does exercise affect the balance of cells in these different states?
The study, published in Molecular Metabolism and led by Wu Tsai Human Performance Alliance graduate student Yotam Voskoboynik, addressed this question by analyzing data from 75 exercise-related gene expression datasets, covering a range of exercise types, tissue samples, species, and sequencing methods.
The findings reveal that immediately following exercise, your body activates M1 pro-inflammatory macrophages. However, with consistent long-term exercise, your body shifts toward activating M2 macrophages. The study also found variability in the strength of macrophage polarization responses. Females, younger individuals, and those engaging in higher-intensity exercise showed stronger M1 and M2 macrophage activation than males, older adults, and participants in lower-intensity workouts.
“Our findings are significant because macrophage polarization is linked to a variety of human diseases, including cancer, cardiovascular disease, and autoimmune disorders,” write the team. “It suggests that an imbalance between pro-immune and cell repair responses could pave the way for disease development while the balance between the M1 and M2 macrophages is essential for optimal health.”
Importantly, reduced exercise reversed the M1 and M2 effects. The team suggests understanding this process could one day lead to personalized exercise programs to improve health and manage disease. The database of all 75 datasets included in this study is publicly available.
The team also identified a new set of 25 genes that more accurately reflect macrophage polarization in muscle tissues, compared to the existing model that utilizes 338 genes. This smaller set, called the Signature of Muscle Resident Macrophage Polarization, allows for a deeper and more precise study of macrophage behavior in muscles. It also makes it possible to study macrophage polarization with existing exercise and muscle datasets that were not designed for this purpose, expanding the research possibilities in this field.
This work is part of our Multiscale Athlete moonshot to synthesize experimental data across biological scales to predict molecular and cellular states and their effects on whole body performance. The research was co-funded with the National Institutes for Health (NIH).
Co-authors include Andrew D. McCulloch and Debashis Sahoo.
Latest News
January 7, 2026
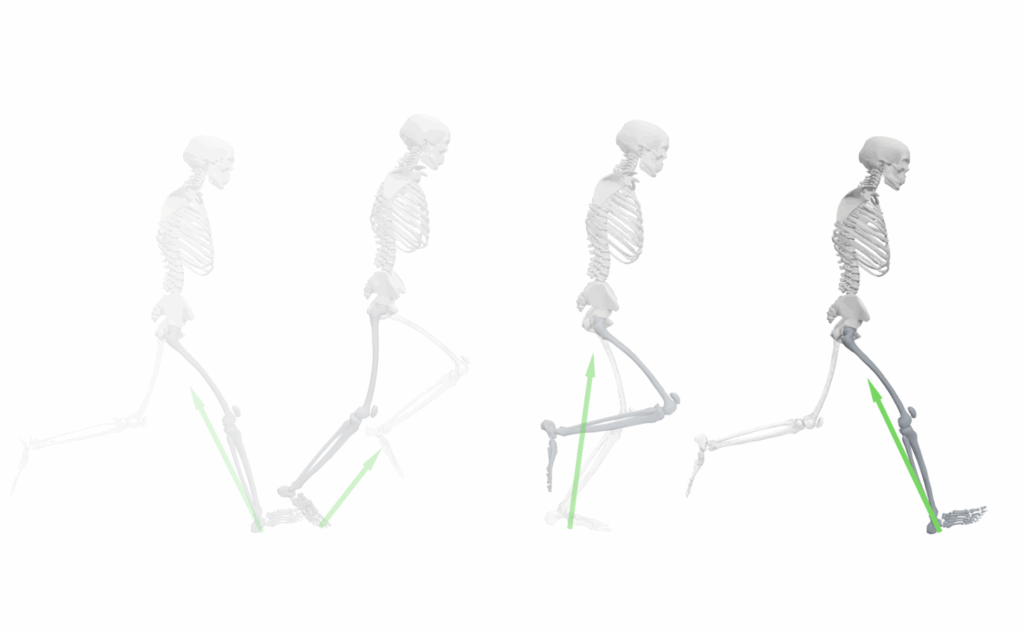
Foundation AI model is transforming analysis of walking and running dynamics

December 10, 2025
Study suggests how eccentric resistance exercises might strengthen tendons

November 21, 2025
Recordings Now Live: Female Athlete Research Meeting 2025
Get Engaged
Join our mailing list to receive the latest information and updates on the Wu Tsai Human Performance Alliance.
